It’s 2022, and eye care practitioners worldwide are prescribing myopia management interventions to reduce myopia progression in children and teenagers.
In most professional circles, myopia is no longer viewed as simply a refractive error but as a precursor to changes in axial length that potentially may result in debilitating visual loss.
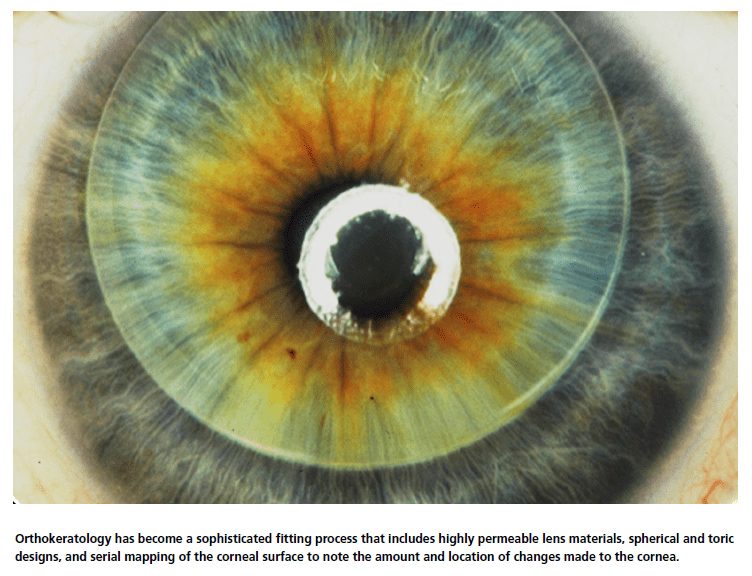
Myopia management has many paths, including orthokeratology (OrthoK), soft lens multifocals, pharmaceuticals, and innovative spectacle lenses. OrthoK is the process of reshaping the cornea to temporarily reduce refractive error. There are scores of OrthoK lens designs marketed across the globe, including from three of the top four soft lens companies. Their use is taught in all academic institutions to optometrists (and many ophthalmologists) in training. It has become a sophisticated fitting process that includes highly permeable lens materials, spherical and toric designs, and serial mapping of the corneal surface to note the amount and location of changes made to the cornea — all aiding to provide predictable outcomes with few complications.
The path that OrthoK has taken to come to its current state is an exciting journey with many twists and turns. There were early attempts to reduce corneal curvature, including the ancient Chinese use of sandbags on the eyes at night to flatten the cornea. A novel invention created by Dr. J. Bell in 1850 was an eye cup with a spring-mounted plunger to pound the cornea flat through the closed eye. These early attempts to flatten the cornea had limited (if any) traction and have nothing in common with what we know today as OrthoK.
Early Design Development
By the mid-20th century, the understanding of the physiology of the eye had been well established, particularly related to the need for oxygenating the cornea. This period was also the beginning of the transition from large diameter sclerals to corneal lenses. Coinciding with this, after World War II, polymethylmethacrylate (PMMA) became the material of choice for contact lenses. While PMMA provided excellent optics and machining capabilities, its non-permeable nature caused corneal edema, resulting in steepening of the corneal curvature. Additionally, if these lenses were inadvertently fitted too flat, the cornea was reshaped, and patients were noting that they were seeing better without their eyeglasses than ever before.
From these observations, interest in the discipline of the planned reshaping of the cornea began to generate more scientific interest. George Jessen (co-founder of Wesley-Jessen Corporation) described a process he called “orthofocus” at a watershed 1962 contact lens specialists conference in Chicago.1 Part of his description was that the base curve (BOZR) of his design would be fitted flatter than the flat keratometry (K) reading by an amount equal to the amount of myopia targeted for the temporary reduction, which went on to be known as the Jessen Factor. At the same conference, his business partner, Newton Wesley, proposed that much research needed to be done, while also suggesting that “orthokeratology” 2 was better terminology to be used. Although there have been many attempts to use another branding for this category, the term remains in place today around the world. The lens designs used at this time, and for many years to come, were standard spherical lenses worn during daytime hours and fit by either using the Jessen method or by employing a series of progressively flatter lenses to alter the corneal shape.
The following two decades widened the interest as early adopters of OrthoK began to publish their works, i.e., May and Grant,3,4 Nolan,5 Freeman,6,7 Kerns,8,9 Polse, et al.,10 and Coon.11 Although there was individual variability and poor predictability, these early adopters demonstrated a modest temporary reduction in myopia (approximately 1.00D to 1.50D). Additionally, unwanted induced astigmatism often was present due to poor lens centration. An example of lens designs from this time is in Figure 1. A patient with -1.50D correction would be fitted 1.50D flatter than the flattest K. The fluorescein pattern shows this flat fit with central bearing and excessive edge lift, demonstrating an unstable fitting relationship and accompanying decentration. The tear profile demonstrates the fitting relationship as well.
Beyond Keratometry
Until this time, contact lens fitting of all types, including OrthoK, was primarily based on manual keratometry and spectacle refraction. This began to change in the late 1970s when along with others, Sami El Hage, OD, PhD, described the use of “Photokeratoscopy and Controlled Keratoreformation” (CKR),12 his term for OrthoK. Topography provided the ability to graphically document the curvature of the cornea both as a baseline and post-fit to compare the impact of the Or thoK fit. (Figure 2)
This technique provided graphical documentation of the impact of contact lens wear by comparing baseline and post-fit images and would go on to become standard of care in years to come.


Reverse Geometry
Al Fontana described a “One-Piece Recessed Optic Design,” where the lens had a posterior optic zone of
6.00mm and fitted 1.00D flatter than the flattest K measurement, while the lens periphery was fit on K. (Figure 3) Although this appears to be a reverse geometry lens by description, it isn’t. Sophisticated CNC lathing technology to produce this design was not yet commercially available. In the late 1980s, Richard Wlodyga provided a more detailed description (Figure 4) by designing a lens with a flat base curve radius (BOZR), a reverse curve radius ≥ 1.00D steeper than the base curve, and a 3.00D steeper secondary curve to control centration.
Wlodyga’s three-curve design was interesting, but he could not get it accurately fabricated like Fontana before him. He reached out to Nick Stoyan from Contex Labs. Their association resulted in a commercially viable product – a 9.6mm lens, 6.0mm OZ, with an aspheric peripheral curve 0.50mm wide, and the introduction of a “reverse curve” that tied these curves together. Ultimately, Stoyan patented this design technology.
The Contex lens-fitting philosophy was based on keratometry readings. The initial lens was fitted 1.50D flatter than the flattest K reading, then employing increasingly flatter lenses until the targeted endpoint was achieved. This system was termed “accelerated orthokeratology.”
El Hage also used his topography expertise to aid in the design and fitting of his three-zone CKR lens. Other inventors soon followed. Tom Reim improved upon the reverse zone, and John Mountford employed a tangent periphery rather than alignment curves. At the same time, Roger Tabb, Al Blackburn, John Reinhart, Jim Reeves, George Glady, and Jim Edwards also made additional improvements.
In the early 2000s, numerous design and manufacturing patents related to Corneal Refractive Therapy (CRT) were filed by Jerry Legerton and Bill Meyers. They changed the reverse curve construction to that of a sigmoid curve to alter the sagittal height of the lens.
The Last Three Decades
Daytime wear of OrthoK was recommended well into the 1990s. Stuart Grant proposed what he termed “night therapy and retention”13 as a means of correction for patients who desired freedom from spectacles and contact lenses during the day. He further suggested that this would be convenient, requiring minimal adaptation, as the lens was worn only during sleep. The eyelid pressure from closed eyes would increase effectiveness while possibly retarding myopic progression.
Soft contact lens manufacturers long were enamored with the possibility of extended wear, which led GP material manufacturers to explore this as well. In 2002, the FDA approved Menicon Z gas permeable contact lenses for 30-day continuous wear. Polymer Technology received FDA premarket approval (PMA) for overnight wear of the Boston Equalens II in 2003. Paragon’s HDS materials (60 and 100) received FDA premarket approval for overnight wear in 2002.
OrthoK fitters embraced Grant’s suggestion of overnight wear, and when combined with higher Dk lens materials, this ushered in the era of overnight OrthoK.

As interest increased in OrthoK, eye care practitioners needed a place to share their clinical findings with their peers. The National Eye Research Foundation (NERF) had attracted like-minded ECPs to periodic meetings for years. The Global Orthokeratology Symposium (GOS) held its inaugural meeting in the summer of 2002. Over 350 practitioners from 30 countries and approximately 20 exhibitors were in attendance. The meeting was held in Toronto, Ontario, Canada, because OrthoK was not an FDA-approved category in the U.S. at that time. Additionally, the meeting organizers were interested in gaining insight from Asian participants during a time when their travel to the U.S. was more restricted.
Among the many highlights of the conference was a session where the different country attendees met among themselves to discuss the formation of their own OrthoK associations, which many did in the U.S. and internationally. The GOS conference was held annually over the next few years before morphing into what is now the Global Specialty Lens Symposium (GSLS). In an oddity reminiscent of today, the 2003 GOS was canceled due to the SARS outbreak, where citizens of countries outside of Canada were temporarily not allowed to travel into the country.
Regulatory Approvals
In January 2002, Paragon Sciences received FDA panel approval for overnight corneal reshaping with the Paragon CRT Lens for patients with myopia between -0.50D to -6.00D and astigmatism up to 1.75D. Ultimately, it had no age restrictions, which would become quite valuable in years to come. In June 2004, the panel approved the Bausch & Lomb Vision Shaping Treatment (VST) for overnight OrthoK using Boston Equalens II. Later that year, B&L received supplemental approval for OrthoK fitting using topography and software. The initial VST lens designs were the BE Retainer, Contex OK, DreamLens, and Euclid Emerald.

Interestingly, they were available only in red and yellow colors, which served a dual purpose. It allowed the patient to differentiate between the right and left lens easily. Additionally, it was a method of tracking the VST design use, as there was an agreement among the different patent holders to share royalties. Presently, there are a dozen different designs marketed under the VST approval.
The construction of OrthoK designs continued to morph as innovators with four to five curves (or zones) (Figure 5) attempted to improve fitting characteristics.
The Orthokeratology Handbook
Roger Kame and Todd Winkler published The Orthokeratology Handbook14 in 1995, describing in detail the new accelerated OrthoK process and introduced the term “reverse geometry lenses.” This resource did an excellent job of providing real-life case histories, including corneal topographies.

John Mountford et al. penned Orthokeratology Principles and Practice,15 in what remains today a valuable asset for the aspiring orthokeratologist, providing insight on fitting, lens design, baseline, and post-fit topography for the OrthoK candidate.

The science of OrthoK evolved as well. Swarbrick et al. described the corneal response to overnight OrthoK in numerous papers.16,17 Cho and the Hong Kong Polytechnic team studied myopia progression reduction with OrthoK,18,19 toric OrthoK designs,20 the validity of the Jessen Factor,21 and more. Nichols et al. looked at the patient response in overnight OrthoK.22 Since the early 2000s, hundreds of peer-reviewed publications have been published on this topic, with scores of studies in progress. Most of the recent OrthoK publications emanate from Asia. These are often large-scale studies involving hundreds of wearers, as Asia, and China in particular, has seen the use of OrthoK for myopia control performed on millions of eyes.
New developments continue as empirical fitting has become refined, topography-based designs with software manipulation of parameters increase in popularity, and the use of asymmetrical back surfaces is more widely accepted. Designs with five to six curves or zones (Figures 6a and 6b) and small optic zones may lead to even better overall fitting of OrthoK and expanded use in eye care practices around the globe.
References
1 Jessen GN. Orthofocus techniques. Contacto 1962;6:200–4.
2 Nolan JA. Flashback: the first ortho-k meeting. Contacto 1995;38:9–1
3 May and Grant. Orthokeratology-control of refractive errors through contact lenses. J Am Optom Assoc, 42 (1971), pp. 1277-1283.
4 Grant, S.C. and May, C.H. Effects of corneal curvature change on the visual system. Contacto, 16, (2), 65-69 (1972).
5 Nolan, J.A. Orthokeratology with steep lenses. Contacto, 16, (3), 31-37 (1972)
6 Freeman 1978 Freeman, RA. Predicting stable changes in orthokeratology. Contact Lens Forum, 3, (1), 21-31 (1978).
7 Freeman, RA. Predicting stable changes in orthokeratology. Contact Lens Forum, 3, (1), 21-31 (1978).
8 Kerns, R.L. Research in orthokeratology. Part I: introduction and background. ]. Am. Optom. Assoc., 47, 1047-1051 (1976).
9 Kerns, R.L Research in orthokeratology. Part VIII: results, conclusions, and discussion of techniques. J. Am. Optom. Assoc., 49, 308-314 (1978).
10 Polse, K.A., Brand, RJ., Schwalbe, J.S., Vastine, D.W. and Kenner, R. J. The Berkeley orthokeratology study. Part II: efficacy and duration. Am. J. Optom. Physiol.
Opt. 60, 187-195 (1983).
11 Coon, L.J. Orthokeratology: Part II: evaluating the Tabb method. Am. Optom. Assoc., 55, 409-418 (1984).
12 El Hage S. Photokeratoscopy and Controlled Keratoreformation. Paper presented at the International Symposium of Ophthalmological Optics; May 7–9,
1978; Tokyo, Japan
13 Grant, S. Orthokeratology night therapy and retention. Contacto, 35, (June), 30-33 (1995).
14 The Orthokeratology Handbook; D. Todd Winkler and Rodger T. Kame. ISBN 0 7506 9595 1 Published by Butterworth-Heinemann, 1995.
15 Orthokeratology: Principles and Practice: J. Mountford, D. Ruston, Trusit Dave. ISBN 978-0-7506-4007-7 Published by Butterworth-Heinemann, 2004
16 Swarbrick Helen, Wong G, O’Leary DJ. Corneal response to orthokeratology. Optom Vis Sci (1998) Nov;75(11):791-9.
17 Swarbrick Helen. Orthokeratology (corneal refractive therapy): what is it and how does it work? Eye Contact Lens. 2004 Oct;30(4)
18 Lui Wai-On, Edwards Marion, Cho Pauline. Contact lenses in myopia reduction – From orthofocus to accelerated orthokeratology. Contact Lens & Anterior
Eye (2000)
19 Cho Pauline, Cheung, Sin Wan, Edwards Marion. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive
changes and myopic control Curr Eye Res (2005) Jan;30(1):71
20 Cheung Sin Wan, Cho Pauline, Chan, Ben. Astigmatic Changes in Orthokeratology. (2009). Optometry and Vision Science.
21 Chan Ben, Cho Pauline, Mountford, John. (2008). The validity of the Jessen formula in overnight orthokeratology: A retrospective study. Ophthalmic
& physiological optics
22 Nichols JJ, Marsich MM, Nguyen M, Barr JT, Bullimore MA. Overnight orthokeratology. Optom Vis Sci. (2000) May;77(5):252-9